Vermont Occupational Safety and Health Administration has released a pre-citation settlement agreement regarding the September 2015 death of Trooper Kyle Young.
According to the report, VOSHA found two violations that did not contribute to Young’s death.
If the Department of Public Safety provides the Department of Labor with a draft comprehensive safety plan by July 1, it will not be cited for the trooper’s death.
Young, 28, collapsed while trying out for the Vermont State Police Tactical Services Unit at the Ethan Allen Firing Range in Jericho on September 17, 2015.
He was pronounced dead at the UVM Medical Center. His cause of death was exertional heatstroke.
The temperature the day of his death was approximately 82 degrees.
“It was like military gear,” said Denise Alosa, describing what Young was wearing when he collapsed.
Denise Alosa and Dr. Suzanne Elliott consulted with VOSHA on the investigation into his death.
They are both medical coordinators for the Vermont City Marathon.
The marathon has seen 26 cases of exertional heatstroke. Everybody has survived.
“Because we were trained and had seen it…we reached out to them and they reached out to us,” said Alosa.
Her takeaway from what happened to Kyle Young: the need for training.
“If you haven’t been trained to recognize it early, many people get it confused with other things,” said Alosa.
One VOSHA violation was due to a lack of a written respiratory program. It was an ancillary finding, and “not associated directly with the investigation into Kyle Young’s death,” the report reads.
Another violation was regarding first aid. While trained first aid responders were on site, “given the nature of the physical activity, the industry standard requires that ice packs or other cooling devices be available,” according to the report.
“The big thing with exertional heatstroke, the big kind of tag line is ‘cool first. Transport second’,” said Alosa.
While VOSHA does not attribute either of these violations to Young’s death, it is requiring the Department of Public Safety to provide a draft safety plan by July 1 to avoid citations.
That department began reevaluating its procedures soon after Young’s death.
“This is a process. It’s not an event so it’s still moving forward,” said Public Safety Commissioner Keith Flynn in an interview late last week.
State Police have recommended training in heat stroke and heat-related injuries, a hydration schedule and wet bulb globe temperature monitoring to monitor the climate before and during physical tests.
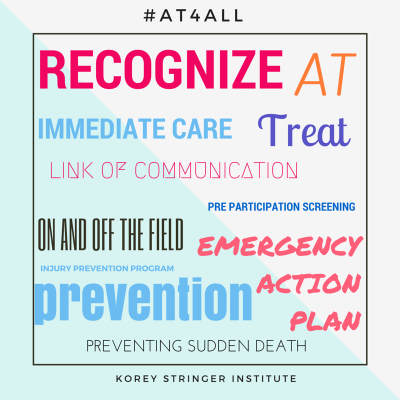
“We’ve just entered into a contract with the Korey Stringer Institute so We’re going to have some of the top experts in the country really take a look at our programs so that we make sure we have good programs in place,” said Commissioner Flynn.
In a statement from Flynn Monday, he said “VOSHA acknowledged the Department’s commitment to improving its training and physical testing protocols to better protect its members… The Department is committed to reviewing and improving its testing protocols to protect its members to the greatest extent possible…”
The Department of Labor declined a request for an interview.
Source: myChamplainValley.com