WHAT PUTS AN INDIVIDUAL AT RISK FOR ASTHMA?
As asthma is a disease which may be developed at any time in life, the risk factors presented here describe not only the risk of having an asthmatic episode, but also those which influence the development of the disease.
| Intrinsic Risk Factors | Extrinsic Risk Factors |
| Genetics | Allergens (Indoor and Outdoor) |
| Family History of Asthma | Respiratory Illnesses (Mostly Viral) |
| Obesity | Time of Day (Early Morning or Night Time) |
| Males | Poor Asthma Control |
| Medications (NSAIDS or Aspirin) | |
| Cold Weather | |
| Environment (Smoke, Dust Mites, Pollution) |
HOW CAN YOU PREVENT ASTHMA?
- Early recognition of the condition
- Control of the disease
- Take breaks as needed
- Avoid aggravating activities
LOOK FOR THESE SYMPTOMS IN ATHLETES WHEN ASTHMA IS SUSPECTED:
INITIAL DIAGNOSIS
Recognition of signs and symptoms commonly lead the athlete to seek medical advice.
Note: diagnoses made using a bronchodilator should only be performed by a physician.
Signs and symptoms may include:
| Episodic Breathlessness | Wheezing |
| Coughing | Chest Tightness |
| Difficulty Speaking in Full Sentences | Shortness of Breath |
| Drowsiness | Confusion |
| Use of Accessory Muscles for Breathing | Measure Lung Function |
FORCED EXPIRATORY VOLUME (FEV)
- Measurement of the amount of airflow in the first second of expiration
- Diagnosis of asthma at < 40% FEV
- If a bronchodilator increases FEV by 12%, asthma may be diagnosed.
| Severity of Obstruction | Mild | Moderate | Severe | Very Severe |
| Percent of Forced Expiratory Volume | 70-99% | 50-69% | 35-49% | < 35% |
PEAK EXPIRATORY FLOW RATE (PEFR)
- May be used to diagnose (but not preferred) and monitor management of asthma
- Peak Flow Meters are commonly inexpensive, portable, an easy to use
- Because of the large range of scores, PEF score can only be compared to the patient’s own best score
- Diagnosis of asthma at 20% improvement after bronchodilator use
These methods may also be used in conjunction with common allergens or triggers to determine individual sensitivities for prevention of asthmatic episodes.
EPISODIC DIAGNOSIS
Diagnosis of an asthma episode or “attack” is primarily based on signs and symptoms. Signs and symptoms may include:
- Episodic breathlessness
- Wheezing
- Coughing
- Chest tightness
- Difficulty speaking in complete sentences
- Shortness of breath
- Drowsiness
- Confusion
- Use of accessory muscles for breathing
As an athlete is restricted of oxygen from breathing difficulty, the possibility of loss of consciousness or other mental status changes becomes more imminent.
WHAT ELSE COULD THIS BE?
- Upper Airway Obstruction
- Inhaled Foreign Body (Choking)
- Exercise-induced Bronchospasm
- Anaphylaxis
- Vocal Cord Dysfunction
- Anxiety and Panic Attack related Hyperventilation
- Spontaneous Pneumothorax
- Other forms of Obstructive Lung Disease (primarily COPD)
- Symptoms may also have non-respiratory causes (left ventricular failure)
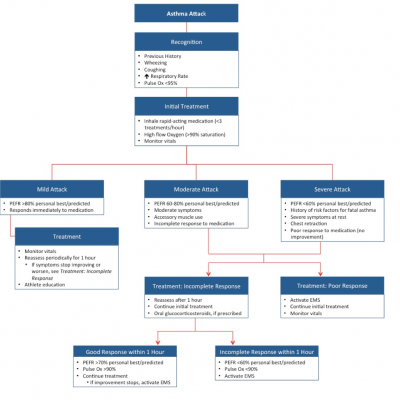
Follow this algorithm to determine diagnosis and treatment options:
HOW DO YOU TREAT SOMEONE WITH ASTHMA?
Medications may be delivered by several methods: inhaled (most common), oral, or via injection. Treatment can be used to establish control of asthma, which is a daily treatment, or to relieve the symptoms of asthma as they occur.
CONTROL (DAILY)
- Avoidance of triggers and allergens
- Use of controller medication, as prescribed
Controller Medications may include:
| Inhaled glucocorticosteroids | Leukotriene modifiers |
| Long-acting inhaled bronchodialators | Theophylline |
| Cromones | Long-acting oral beta-agonists |
| Anti-IgE | Systemic glucocorticosteroids |
| Oral anti-allergic compounds | Allergen-specific immunotherapy |
Clinical Control of Asthma is defined as:
- No daytime symptoms (≤ 2 times per week)
- No limitations of daily activities, including exercise
- No nocturnal symptoms
- No need for reliever treatment (≤ 2 times per week)
- Normal or near-normal lung function
- No exacerbations
LEVELS OF ASTHMA CONTROL
- Assessment of current clinical control (preferably over 4 weeks)
| Characteristic
|
Controlled
(All of the following must be present)
|
Partially Controlled (Any measure present) | Uncontrolled |
| Daytime Symptoms
|
Few to none (twice or less per week) | More than twice per week | 3+ features of partially controlled asthma*† |
| Limitation of Activities
|
None | Any | |
| Nocturnal Symptoms or Awakenings | None | Any | |
| Need for Reliever/
Rescue Treatment
|
Few to none (twice or less per week) | More than twice per week | |
| Lung Function
(PEF or FEV1) ‡
|
Normal | < 80% predicted or personal best (only if known) |
Adapted from Fitzgerald, 2013. Any exacerbation should prompt review of maintenance treatment to ensure that it is adequate. Lung function is not a reliable test for children 5 years old or younger.
† By definition, an exacerbation in any week makes that an uncontrolled asthma week
‡ Without administration of bronchodilator
- Assessment of Future Risk (risks of exacerbations, instability, rapid decline in lung function, other side-effects)
Features that are associated with increased risk of adverse events in the near future include:
- Poor clinical control
- Frequent exacerbations in the past year*
- Admission to critical care for asthma
- Low FEV1
- Exposure to cigarette smoke
- High dose medications
To gain control of asthma, the Global Initiative for Asthma recommends a 3-pronged approach:
- Develop a patient/medical care provider partnership
-
- Education on asthma management and treatment
- Personal written asthma action plan to help individuals respond to their asthma appropriately
- Identify risk factors and reduce exposure to risk factors,
-
- By avoidance or medication
- Assess, treat, and monitor asthma
-
- Treat to achieve control
- Monitor to maintain control
RELIEF (ASTHMA ATTACK)
Treatment should be administered based on the severity of the asthma attack. Below is a table which outlines the severity of asthma based on several factors. Some of these factors can be used in the field, however during exercise breathing and heart rates may already be increased.
- Cessation of activity
- Administration of relief medication via a metered-dose inhaler (MDI) ideally with a spacer
- For mild to moderate attacks, bronchodilator use is called for
- Bronchodilators should be used as prescribed (generally 2-4 puffs every 20 minutes for the first hour of discomfort)
SEVERITY OF ASTHMA SYMPTOMS:
| Symptoms
|
Mild Asthma | Moderate Asthma | Severe Asthma | Respiratory Arrest Imminent |
| Breathless while…
|
Walking | Talking | At Rest | |
| Position
|
Can lie down | Prefer Siting | Hunched Forward | |
| Talking Ability
|
Sentences | Phrases | Words | |
| Alertness
|
May be agitated | Usually agitated | Usually agitated | Drowsy/
confused |
| Respiratory Rate
|
Increased | Increased | > 30 breaths/min | |
| Accessory muscles used and suprasternal retractions | Usually Not | Usually | Usually | Paradoxical thoraco-abdominal motion |
| Wheeze | Moderate, often only at the end of expiration | Loud | Usually Loud | Absence of wheeze |
| Pulse (beats/min)**
|
<100 | 100-120 | >120 | Bradycardia |
| PEFR after initial bronchodilator administration*** | > 80% | 60-80% | <60% |
Adapted from Fitzgerald, 2012. Note: the presence of several parameters, but not necessarily all indicates the general classification of severity
* Respiratory rate may be elevated due to exercise, look for decreased rate with rest
**Pulse may be elevated due to exercise, look for decreased rate with rest
*** PEF % of predicted or personal best
IF DISCOMFORT DECRREASES BUT REMAINS:
- Mild attack may require 2-4 puffs every 3 to 4 hours
- Moderate attack may require 6-10 puffs every 1 to 2 hours
- Check pulse oxygen (O2) with a pulse oximeter
- Administer supplemental O2 if, pulse O2 drops below 95%
- Check and monitor PEFR after bronchodilator use
- Activate EMS if symptoms do not improve
- Prepare for rescue breathing and CPR after EMS is activated
RECOMMENDED LIST OF MATERIALS
- Controller inhaler (for everyday use)
- Rescue inhaler
- Spacer if available (improvise with tape roll)
- Peak flow meter
- Stethoscope
- Supplemental oxygen
- Bag-valve mask/pocket-mask
- Non re-breather mask
- Pulse oximeter
REFERENCES
- Global Strategy for Asthma Management and Prevention 2012 Update. Retrieved from: http://www.ginasthma.org/documents/4. Accessed July 2013.
- Miller MG, Baker RJ. Asthma. In: Casa DJ, ed. Preventing Sudden Death in Sport and Physical Activity. Sudbury, MA: Jones and Bartlett Learning. 2012:169-183.
- Miller MG, Weiler JM, Baker R, Collins J, D’Alonzo G. National Athletic Trainers’ Association position statement: management of asthma in athletes. J Athl Train. 2005;40(3):224-245.
- National Heart Lung and Blood Institute. What Is Asthma? http://www.nhlbi.nih.gov/health/dci/Diseases/Asthma/Asthma_WhatIs.html. Published February 1, 2011. Accessed September 2011.
- National Federation of State High School Associations. Sports Medicine Handbook. 2011. 4th ed. Indianapolis, IN: National Federation of State High School Associations.