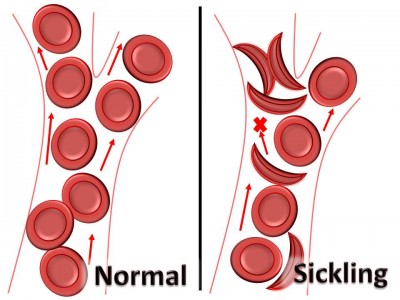
Exertional sickling is a medical emergency occurring in athletes carrying the sickle cell trait. When the red blood cells(RBC) change shape or “sickle” this causes a build up of RBCs in small blood vessels, leading to decreased blood flow. The drop in blood flow leads to a breakdown of muscle tissue and cell death, known as fulminant rhabdomyolysis.
How do you prevent exertional sickling?
- Screen all athletes for sickle cell trait and counsel athletes who are identified as having the trait
- Mandate Preparticipation exams to ensure athletes are healthy for activity
- Acclimatize all athletes by slowly increasing intensity when conditioning or lifting
- Modify drills for sickle cell trait athletes by avoiding timed runs and implementing breaks between runs
- Have water readily available during all activity
- Limit activity if any type of illness is present
- Educate athletes, parents, and coaches about the signs, symptoms, and treatment of exertional sickling
- Be aware of predisposing factors:
- Sickle cell trait
- Heat
- Dehydration
- High altitude
- Asthma
- Illness
- Unacclimatized
- High intensity exercise with short rest intervals
Look for these symptoms in athletes when exertional sickling is suspected:
| Common Signs and Symptoms of an Exertional Sickling episode |
| CrampingMuscle weakness that exceeds muscle pain
Athlete “slumps” to the ground rather than a sudden collapse (rules out cardiac) Able to speak Muscles look and feel normal (rules out heat cramps) Rapid breathing, but pulmonary exam reveals normal air movement (rules out asthma) Rectal temperature less than 103oF (rule out heat stroke) |
Adapted from: Eichner, ER. Sickle cell considerations in athletes. Clin Sports Med. 2011;30:3:537-549.
Exertional sickling is most common when exercise is high intensity and has short or small amounts of recovery time between drills. Sports settings common for exertional sickling collapse are:
- Football conditioning
- Basketball training
- Cross-country racing
- University track tryout
- Golden Gloves boxing bout
What else could this be?
- Exertional heat illness
- Dehydration
- Heat syncope
- Asthma attack
- Cardiac conditions
How do you treat an individual with exertional sickling?
- Stop activity
- Check vital signs (Heart rate, blood pressure, breathing)
- Activate Emergency Medical Services and prepare for CPR
- Administer high-flow oxygen (15L/min)
- Cool athlete if necessary
- Call ahead to hospital and tell staff to expect explosive rhabdomyolysis
- Extended care will be needed to assess body damage (kidneys, liver, etc.)
When can the individual return to activity?
- Physician clearance
- Gradual return to play based on level of sickling and severity of symptoms.
Recommended equipment list
- Emergency action plan
- Cell phone
- Supplemental oxygen
- Rectal thermometer
- Blood pressure cuff and stethoscope
- Wrist watch
Click here to learn more about exertional sickling from the NCAA video
References
- National Athletic Trainers’ Association consensus statement: sickle cell trait and the athlete. National Athletic Trainers’ Association. 1-5.
- Eichner, ER. Sickle cell considerations in athletes. Clin Sports Med. 2011; 30:3,537-549.
- Eichner ER. Pearls and pitfalls: exertional sickling. Curr Sports Med Rep. 2010;9:3-4.
- Eichner ER, Anderson S. Exertional Sickling. In: Casa JD, ed. Preventing Sudden Death in Sport and Physical Activity. Sudbury, MA: Jones & Bartlett Learning; 2012;131-141.
- McGrew CA. NCAA football and conditioning drills. Curr Sports Med Rep. 2010;9:185-186.