By Rachel Katch, Assistant Director of Research
Exertional hyponatremia (EH) is a rare, yet potentially fatal condition that is associated with a serum sodium concentration less than 130mEq/L. There are two common causes for this lack of sodium in the blood, which are: (1) an individual ingests fluid replacement beverages well beyond sweat losses, and (2) an individual’s sodium losses through sweat are not replaced adequately. There are many risk factors for developing this condition, but a few key factors are overhydration, participating in events that last longer than four hours, and gender. Many individuals think that the more fluid they ingest, the better for their body it is during exercise. This is not always the case. By over hydrating, you are setting yourself up for EH due to sodium depletion. Secondly, by competing in exercise greater than four hours, an individual tends to drink more fluid due to the increased time, which would again set them up for sodium depletion both from sweating and overhydrating. And lastly, gender does play a role. EH is more commonly found in females due to their generally small stature. The theory is the smaller the body mass index, the more effect overhydrating will have on the body due to having a smaller mass to dilute.
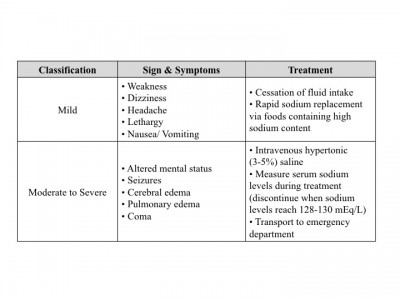
The signs and symptoms, as well as treatment, of EH are outlined in Table 1. Mild symptoms generally occur with a serum sodium concentration between 135-130mEq/L. Moderate to severe symptoms start to occur when serum sodium concentrations start falling below 130mEq/L. The lower the sodium concentration, the faster an individual will decline in health, and if they are not treated appropriately EH possibly will result in death due to encephalopathy.
There are many ways to implement prevention strategies to mitigate the risk of suffering from EH, which include but are not limited to: (1) education on fluid intake before, during, and after competition, (2) maintaining a healthy diet that incorporates appropriate sodium intake, and (3) creating individualized fluid replacement protocols. Proper education on hydration is a key feature to preventing EH by letting individuals know what is appropriate so they do not overhydrate. Prior to exercise, an individual would want to be hydrated; but what does that mean? Proper pre-exercise hydration includes consuming 500-600mL of water or sports drink two to three hours before exercising, and then consuming 200-300mL 10-20 minutes before. Appropriate hydration during an event is crucial as well, and generally includes consuming 200-300mL every 10-20 minutes. And lastly, post-exercise hydration aims to correct any fluid loss during exercise by consuming fluid containing water, carbohydrates, and electrolytes within two hours of exercise completion.
Table 1. Exertional Hyponatremia Signs & Symptoms with Treatment
Maintaining a healthy diet that incorporates correct sodium intake for your exercise is also important. Dietary sodium supports normal body maintenance of fluid balance and can help prevent muscle cramps, heat exhaustion, and EH. This is especially important for those individuals exercising in hot weather due to the excess sodium depletion through sweating. It is significant to note that sports drinks generally contain low levels of sodium relative to blood, and should not be the only source of sodium replenishment. Instead, eat salty foods such as soup or pretzels prior to exercise while using sports drink as a supplement the diet.
Lastly, creating individual fluid replacement protocols is the most effective way to prevent EH. An individualized fluid prescription incorporates, but is not limited to, factors such as: (1) sweat rate, (2) sport dynamics (rest breaks, access to fluid), (3) environmental factors, (4) acclimatization state, (5) exercise duration, (6) exercise intensity, (7) gastric emptying/intestinal absorption, and (8) individual preferences. Some individuals sweat more than others; have a slower gastric emptying rate; have different fitness/heat acclimatization status; etc. which all lead to different fluid replacement protocols. These protocols should always be individualized and not generalized to maximize performance and to mitigate the risk of suffering from EH.
Everyone is different, and their fluid replacement protocols should be no exception.